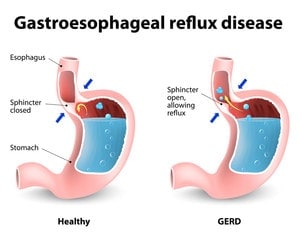
Anti-Reflux Surgery (Laparoscopic Nissen Fundoplication)
Performed for patients with reflux (GORD) disease not controlled with gold standard medical treatment. Surgery performed via a laparoscopic approach in hospital from 2-3 days and full recovery in 6 months.
Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy, often called the "sleeve", is performed by removing approximately 70-80% of the stomach. The remaining stomach is the size and shape of a banana.
The Procedure:
- The stomach is freed from organs around it.
- Surgical staplers are used to remove the stomach, making it much smaller.
How it Works
The new stomach holds less food and liquid helping reduce the amount of food (and calories) that are consumed. By removing the portion of the stomach that produces most of the “hunger hormone Ghrelin”, the surgery has an effect on the metabolism. It decreases hunger, increases fullness, and allows the body to reach and maintain a healthy weight as well as blood sugar control. The simple nature of the operation makes it very safe without the potential complications from surgery on the small intestine.
Advantages
- Technically simple and shorter surgery time
- Can be performed in certain patients with high risk medical conditions
- May be performed as the first step for patients with severe obesity
- May be used as a bridge to gastric bypass or other procedures
- Effective weight loss and improvement of obesity related conditions
Disadvantages
- Non-reversible procedure
- May worsen or cause new onset reflux and heart burn
- Less impact on metabolism compared to bypass procedures
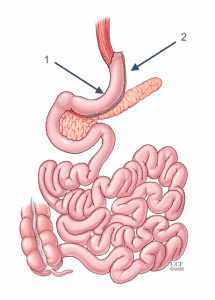
Roux-en-Y Gastric Bypass (RYGB)
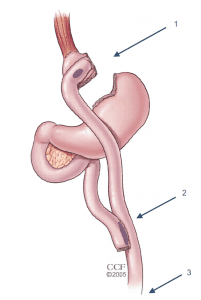
The Roux-en-Y Gastric Bypass, often called the “gastric bypass”, has now been performed for more than 50 years and the laparoscopic approach has been refined since 1993. It is one of the most common operations and is very effective in treating obesity and obesity related diseases. The name is a French term meaning “in the form of a Y”.
The Procedure:
- First, the stomach is divided into a smaller top portion (pouch) which is about the size of an egg. The larger part of the stomach is bypassed and no longer stores or digests food.
- The small intestine is also divided and connected to the new stomach pouch to allow food to pass. The small bowel segment which empties the bypassed or larger stomach is connected into the small bowel approximately 1-1.5 meters downstream, resulting in a bowel connection resembling the shape of the letter Y.
- Eventually the stomach acids and digestive enzymes from the bypassed stomach and first portion of the small intestine will mix with food that is eaten.
How it Works
The gastric bypass works in several ways. Like many bariatric procedures, the newly created stomach pouch is smaller and able to hold less food, which means fewer calories are ingested. Additionally, the food does not come into contact with the first portion of the small bowel and this results in decreased absorption. Most importantly, the modification of the food course through the gastrointestinal tract has a profound effect to decrease hunger, increase fullness, and allow the body to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of adult onset diabetes even before any weight loss occurs. The operation also helps patients with reflux (heart burn) and often the symptoms quickly improve. Along with making appropriate food choices, patients must avoid tobacco products and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen.
Advantages
- Reliable and long-lasting weight loss
- Effective for remission of obesity-associated conditions
- Refined and standardized technique
Disadvantages
- Technically more complex when compared to sleeve gastrectomy or gastric band
- More vitamin and mineral deficiencies than sleeve gastrectomy or gastric banding
- There is a risk for small bowel complications and obstruction
- There is a risk of developing ulcers, especially with NSAID or tobacco use
May cause “dumping syndrome”, a feeling of sickness after eating or drinking, especially sweets
Procedure:
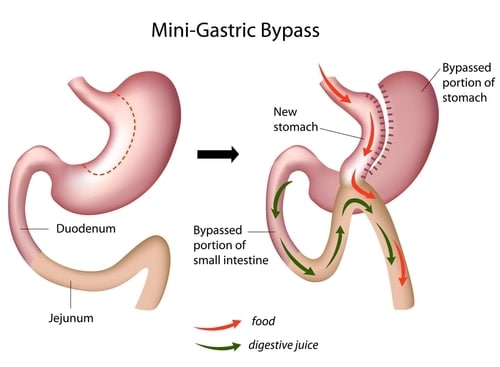
It is also sometimes called Omega Loop Gastric Bypass or One Anastomosis Gastric Bypass.
Surgery is performed under General Anaesthesia using laparoscopic (keyhole) techniques through 5 small incisions in the abdomen.
The surgery is simpler and safer than the Roux en Y but the incisions are the same. The stomach is divided into a long thin pouch, and then a loop of bowel is brought up and joined to it. The main benefit of this procedure over the traditional RYGB is one small bowel anastomosis rather than two.
Digestive juices travel without food to act on until they come to the loop up at the stomach.
Food digestion only happens in the lower part of the small intestine. Food will now move through the new tube stomach into the attached loop of jejunum.
A potential disadvantage is that if ‘reflux’ occurs it will contain some digestive juices that can damage the oesophagus. It is therefore not ideal for patients with severe reflux, nor for smokers.
This surgery is increasingly performed as it has less problems of obstruction and acid reflux than a sleeve, with more powerful weight loss and diabetes control.
Like all bypass procedures, there is a need to take multivitamins long term and to have blood tests every year.
Ask Dr John Jorgensen which procedure is best suited to your situation.
Hernias
Hernia repair involves a surgical correction of a hernia – a bulging of internal organs or tissues through the wall that contains it.
Here are the hernia procedures Dr Jorgensen commonly performs:
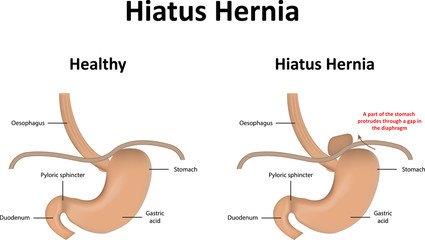
Laparoscopic Hiatal Hernia Repair
- This procedure is for patients where a significant portion of the stomach has herniated into the chest, causing obstructive symptoms such as difficulty in swallowing, early satiety, pain and vomiting or shortness of breath.
- The procedure is done laparoscopically and has a 2-3 day post-operative stay.
- Full recovery takes up to 4 weeks.
Inguinal Hernia
- Inguinal or groin hernias cause bulges along the groin area that may appear to get bigger when you stand up or cough, or may be sensitive to touch.
- Fullness in the groin, sharp pain or pain when exercising, coughing or bending over may be other symptoms.
- They are best repaired with a laparoscopic approach as this results in a rapid recovery.
- Occasionally, open surgery is indicated if previous pelvic surgery has been performed.
- Prosthetic mesh is used for laparoscopic or open repair.
Umbilical/Incisional Hernia
- Smaller (< 5cm) hernias are best approached laparoscopically if possible.
- Larger hernias require open surgery.
- Prosthetic mesh is used with laparoscopic or open repairs.
Stomach Surgeries
Laparoscopic Partial Gastrectomy
- Usually performed for benign or low grade tumours such as lipase or gastrointestinal stromal tumour (GIST)
Open Radical Gastrectomy
- Indicated for gastric cancer after careful patient staging
- Appropriate treatment algorithm based on stage (gastroscopy, CT scan and laparoscopy) and multi-disciplinary cancer meeting assessment
- Patients often have pre-operative chemotherapy followed by surgery
- Surgery is usually open surgery
Laparoscopic sleeve gastrectomy
- In this procedure approximately 80% of the stomach is removed leaving a banana shaped stomach.
- The surgery is done laparoscopically and results in a 2-3 day hospital stay.
- Patients return to work in two weeks.
- Weight loss is rapid and complete in about 12 months.
- The average weight loss is 75% of excess weight.
- The surgery works by restriction (smaller stomach) and gastro-intestinal hormonal changes.
- There is a dampening (reduction) in the hunger hormone grehlin and an increase in satiety hormones such as GLP-1 and PYY.
- The end results in less hunger and earlier satiety with a meal.
Advantages
- Rapid and significant weight loss in 12 months
- No foreign body
- No intestinal surgery
- Both a restrictive and hormonal procedure
- Good quality of eating.
Disadvantages
- Non-reversible
- Potential micronutrient deficiency
- Gastro-oesophageal reflux in 15% of patients
Laparoscopic gastric bypass (RYGB)
- The surgery like the sleeve works with a restrictive component and a gut-hormone component.
- Again, hunger hormones are dampened and satiety hormones enhanced.
- Patients are less hungry and sated with small amounts of food.
- Weight loss is significant and rapid occurring over 12 months.
- The average weight loss is 75% of excess weight.
Advantages
- Long-track record
- Reversible
- Good weight loss
- Good quality of eating
Disadvantages
- Risk of small bowel obstruction
- Risk of stomal ulcer
- Dumping syndrome
- Risk of micronutrient deficiencies
Laparoscopic adjustable gastric band
- Placing an inflatable band around the upper portion of the stomach creating a small gastric pouch above the neck of the stomach.
- The AGB works by reducing hunger.
- The mechanism for this is not well understood.
Advantages
- Very safe to insert
- Short hospital stay (24 hours)
- Reversible
- Low risk of micronutrient deficiencies
Disadvantages
- Slow weight loss
- Poor weight loss in many
- Food intolerance, reflux, vomiting
- Device failure
- High re-operation rate
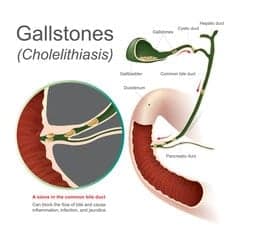
Gallbladder Surgeries
Laparoscopic Cholecystectomy
- Performed for patients with gallstones that are causing pain.
- Occasionally, cholecystectomy is required for polyps of a certain size/shape.
- Rarely cholecystectomy is offered for patients with biliary pain, even in the absence of gallstones.
Choloangiogram
- Choloangiogram is a special x-ray procedure that is done with contrast media to visualize the bile ducts after the a cholecystectomy (removal of the gallbladder). The bile ducts drain bile from the liver into the duodenum (first part of the small bowel).
